
When Olubukola Abiona began a four-year postbaccalaureate fellowship at the National Institutes of Health Vaccine Research Center in 2017, she knew she’d gain valuable experience—but had no idea just how impactful her efforts would be.
Not long later, those impacts became clear: Her team’s research took center stage worldwide as the foundation for vaccines against COVID-19. Their findings were pivotal in the development of not only the Moderna vaccine, but also Pfizer’s, as their previous research supported the discovery of monoclonal antibodies.
And for Abiona—who was featured for her efforts recently by CNN—they only solidified her desire to become a physician-scientist. Now an MD/PhD student at Case Western Reserve University School of Medicine, Abiona spoke with The Daily about her work that helped save millions of lives and changed the course of history.
Laying the groundwork
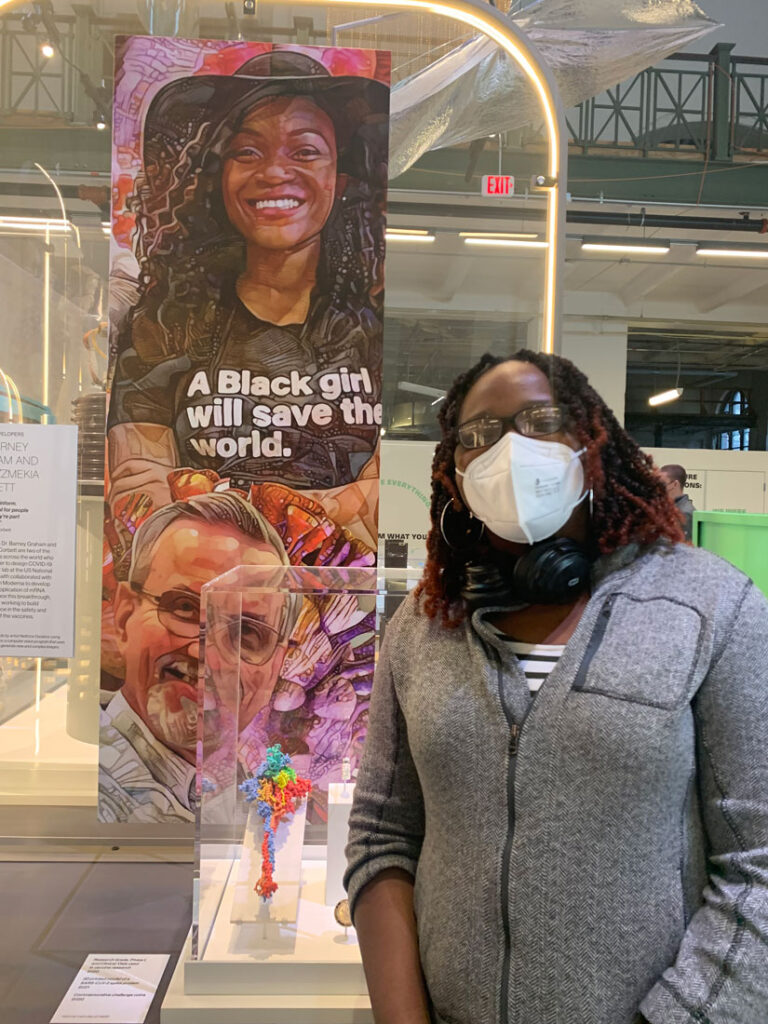
A graduate of the University of Maryland, Baltimore County, Abiona joined the laboratory of the Vaccine Research Center’s director, renowned virologist Barney Graham, working under senior research fellow and immunologist Kizzmekia Corbett. Their focus? Preparing for the possibility of a pandemic driven not by a variant of influenza… but by a coronavirus.
“Dr. Corbett was confident coronavirus was going to be the next big thing,” said Abiona. “Many people didn’t listen to her. They would ask, ‘Who is this person?’”
Corbett’s work reflected a center-wide shift toward pandemic preparedness, marking a change in course from the reactive efforts that drove vaccines for infectious diseases such as Ebola, Middle East respiratory virus (MERS) and severe acute respiratory syndrome (SARS). With Graham’s support, she and Abiona focused their efforts on the possibility of a coronavirus-related outbreak, quietly and methodically building upon virus research that started decades earlier.
“Initially, it was just me and Dr. Corbett [who were] working on coronaviruses,” Abiona explained. “We were a team of two in Dr. Graham’s lab.”
Putting science into action
By the end of 2019, the dynamic in Corbett’s lab shifted—and did so quickly. Rumblings of a virus outbreak in Wuhan, China, were making their way through the center, and it wasn’t long before they reached the group.

“Dr. Graham gathered everyone in the lab to inform them it was time to run the drill—to test the fire alarm,” said Abiona. “We were asked, ‘How fast can we do this? How rapidly can we create a vaccine candidate to combat the new coronavirus?’”
The scenario flew in the face of the typical vaccine and drug development process—one known to be lengthy, expensive, and marked with clinical trials—but Corbett and Abiona were up to the challenge. Joined by research fellows Geoffrey Hutchinson and Cynthia Ziwawo, they put their theories to the test, working schedules Abiona described as “living in a bubble” at the lab.
“Specifically, when we talk about the coronavirus, we are talking about the spike protein; how do we stabilize this virus protein to elicit a better immune response,” explained Abiona. “We started with mice to see if antibodies were produced and, if so, [did] they bind and provide some level of protection?”
Their efforts paid off. Huddled around an assay plate, they waited to see the results late at night, hoping to see a change in color to yellow that would indicate the desired immune response. Not only was there an immune response, but they witnessed a potent one.
“It turned yellow, and then we watched it turn very yellow,” Abiona recalled. “We were elated—we had something.”
According to Abiona, the experience felt surreal—and it’s one for which she’s incredibly grateful.
“Everything aligned perfectly to the point that it was kind of scary because it was all about timing,” she said. “We could have lost two weeks along the way or lost one day here or there. If [COVID-19] had happened a year before, we wouldn’t have had the knowledge or the resources.”
Looking ahead
Today, Abiona works alongside Professor David Wald in his lab at Case Western Reserve University School of Medicine, where they study how cell therapy immunology can be used to treat cancers. In her view, the work holds similarities to her time at the NIH, specifically with regard to the need to think globally about connecting patients with discoveries.
Having completed her first two years of her medical degree and begun the first of her PhD research, Abiona is unsure which field she’ll specialize in for her future career, but plans to learn and absorb as much as she can during her training to make an informed decision.
One of her most pivotal lessons in her academic training thus far? Don’t be afraid to dream big.
“The experience working on the coronavirus vaccine forever changed me in many ways,” she said. “I think a lot about the opportunities provided to me by Dr. Graham and Dr. Corbett and how others may have overlooked me, and I want to carry that forward for others in my future career.”

