Researchers at Case Western Reserve, University of Washington working to gain novel view of cancer, supported by $3.1 million National Institutes of Health grant
Researchers at Case Western Reserve University and the University of Washington expect to gain valuable new insights into highly aggressive prostate cancer by combining artificial intelligence (AI)-powered diagnostic imaging with three-dimensional (3D) tissue imaging.
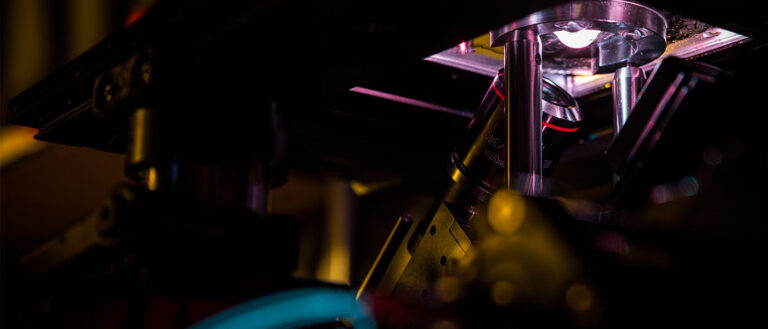
This new AI-3D collaboration will provide a never-before-seen, expanded view and understanding of prostate cancer cells, made possible by a new approach called “light sheet microscopy,” the researchers said. (Seen in photo above by Mark Stone/University of Washington).
Prostate cancer is the most common non-skin cancer in the United States. Doctors will diagnose one in eight men nationally with prostate cancer, and one in 40 will die from the disease, according to the Prostate Cancer Foundation.

Anant Madabhushi, director of the Center for Computational Imaging and Personalized Diagnostics at Case Western Reserve, and Jonathan Liu, a professor of mechanical engineering and bioengineering at the University of Washington (UW), are co-leaders in the new work and will split the funding. The National Cancer Institute (NCI), part of the National Institutes of Health, is supporting the research with a five-year, $3.13 million grant.
“This is an unprecedented meshing of the two most powerful technologies in this area,” said Madabhushi, also the Donnell Institute Professor of Biomedical Engineering at the Case School of Engineering. “We’ll take the AI we’ve developed and, for the first time, be able to apply it to 3D tissue-imaging that the University of Washington excels in—and gain fine, granular detail.”
Identifying aggressive cancer
That fine detail will hopefully reveal even more information about how to identify which prostate cancer cases will be more aggressive in patients, Madabhushi said.
Knowing that could help clinicians determine who would benefit from surgery or radiation therapy—and which patients might be actively monitored instead, he said.
Researchers could also be laying the groundwork to develop what are called “pathomic-based classifiers” of disease outcome for a host of other cancers, Madabhushi said.
Pathomics refers to the application of computer vision and AI to extract a large number of features from tissue images using data-characterization algorithms. The features can then help uncover tumors and other characteristics usually invisible to the naked eye.
Madabhushi’s lab, established in 2012, has become a global leader in the field, specializing in the detection, diagnosis and characterization of various cancers and other diseases by meshing medical imaging, machine learning and AI.
Until now, researchers were using machine learning to focus entirely on two-dimensional images.
“We believe that we’ll be able to train our AI to interrogate 3D tissue images with the same success we have had with two-dimensional images,” Madabhushi said. “But there are so many new possibilities for finding new information in 3D.”
How 3D fits in
Liu and his team have developed a new, non-destructive method that images entire 3D biopsies instead of just a slice. This technique provides full-view images of the tissue and improved predictions of whether the patient had an aggressive cancer.

“With the success of our open-top light-sheet microscopy technologies, an obvious next challenge to overcome was processing and analyzing the massive feature-rich 3D datasets that we were generating from clinical specimens,” Liu said. He said collaborating with Madabhushi’s lab at Case Western Reserve was an “obvious and ideal choice, since developing explainable AI methods will facilitate clinical adoption of a new imaging technology such as ours.”
“This (grant) will help us to scale up our existing collaboration to demonstrate that computational 3D pathology can improve critical treatment decisions for diverse populations of men with prostate cancer,” Liu said.
The 3D images, of course, provide more information than a 2D image. In this case, that means details about the intricate tree-like structure of the glands throughout the tissue.
The advances in 3D technology made by Liu were detailed in a paper published in December 2021 in the journal Cancer Research. Madabushi and three others at Case Western Reserve contributed to the academic paper.
The UW researchers reported in that paper that the 3D features made it easier for a computer to identify which patients were more likely to have cancer return within five years.
Liu had said in a UW news blog that this “non-destructive 3D pathology” would become increasingly valuable in clinical decision-making, such as which patients would require more aggressive treatment or respond to certain drugs.
This new NCI grant complements work supported in an ongoing U.S. Department of Defense grant led by Madabhushi, with Liu as a collaborator. That project combines AI and light sheet-based 3D tissue-imaging technology for studying health disparities in prostate cancer.
For more information, contact Mike Scott at mike.scott@case.edu.
This article was originally published June 21, 2022.