In basketball, to shoot the perfect free throw, train your eye on the rim. In baseball, for the perfect pitch, look at the catcher’s mitt.
So says the “quiet eye” technique, which calls on a period of extended visual attention to improve coordination and performance. A research-backed approach for moments of high stress that require precise motor skills, the technique has been studied not just in athletics, but in operating rooms—places where a surgeon’s “quiet eye” can aid in robot-assisted, minimally invasive surgery.
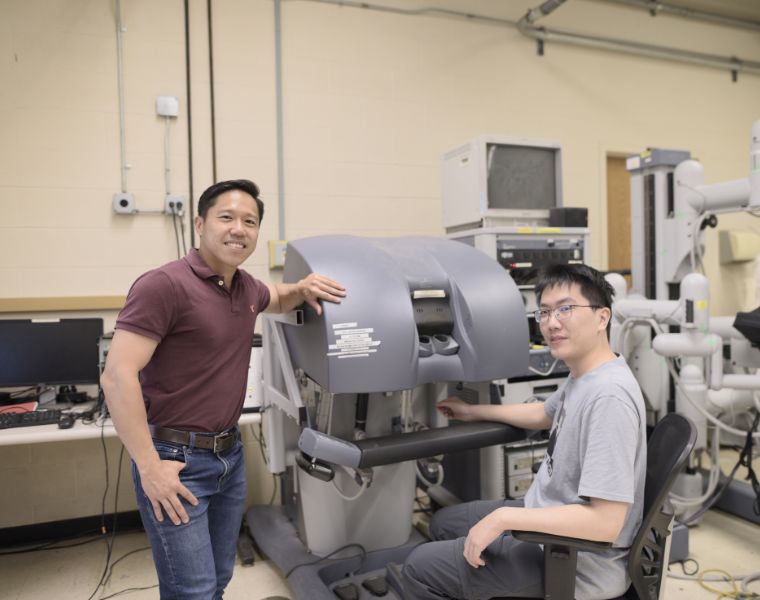
Zonghe Chua, an assistant professor in the Department of Electrical, Computer, and Systems Engineering at Case School of Engineering since 2022, hopes to further advance knowledge of the technique. His project, “Autonomous Gaze Coaching for Robot-assisted Surgical Training,” will be funded by a prestigious National Institutes of Health R21 Trailblazer award, a program that supports new and early career investigators. Totaling $586,000, the three-year grant will help Chua capture the expert gaze and develop more effective surgical training.
A forward focus
With his NIH grant in hand, Chua has a specific focus: “What does it truly mean to be able to perceive a surgical scene like an expert?”
“We are trying to boil that down into an algorithm or a computational model,” he explained, noting how robotic surgery platforms can be difficult to control because, while they mimic hand movements, it’s not exactly one to one—so it can take a while to become proficient in performing procedures using these robots. He hopes to reduce that learning curve, building on existing evidence that has found that teaching junior surgeons where to look helps them improve their control of a robotic surgery platform.
“The project here is really about capturing this expert vision,” Chua said, “and seeing if we can show some kind of teaching aid to novice surgeons, who are still learning how to use the robot.”
During robot-assisted surgery, a surgeon looks into the body through an endoscopic camera that uses two cameras to provide the surgeon with 3D vision inside the patient’s body. Within that surgical tool, Chua plans to use gaze tracking technology—similar to modalities in virtual reality headsets.
He’ll partner with University Hospitals Urology Institute to conduct this research, which involves three main steps. First, the team will measure what it means to be an expert versus a novice surgeon. Then, they’ll work to develop a computational model of expert gaze. Finally, they’ll test whether the system works on novices to improve their skill.
“Surgical expertise is rare,” Chua said. “It’s a precious resource, but if you can capture this as a computational model that you can then display to surgeons to develop their expert gaze, then you increase accessibility to surgical expertise, especially during training.”
Optimizing surgical approaches
Expert surgeons’ time is often limited; they’re needed in operating rooms and in high demand to train the next generation of surgeons.
By quantifying their expertise and training the computational models, “certain aspects can be democratized or made more accessible, even to other institutes,” Chua said. An autonomous coaching system would also be an important step toward lowering the cost of surgical instruction.
Chua is grateful for the collaborative research environment at Case Western Reserve.
“The [CWRU] community is a really good place to do biomedical driven research,” he said. “The department and the whole community—within the engineering department in the School of Engineering and the electrical engineering department— that expertise right—is what really allowed me to succeed in this initial part of my career to get [the NIH Trailblazer award].”