Quick and automated count of tubules correlates with current best—but expensive— genomic test determining who needs chemotherapy and who doesn’t
The number of tubules in tumors may predict which women with estrogen receptor positive (ER+) breast cancer will benefit from hormone therapy alone and which require chemotherapy, researchers at Case Western Reserve University have found.
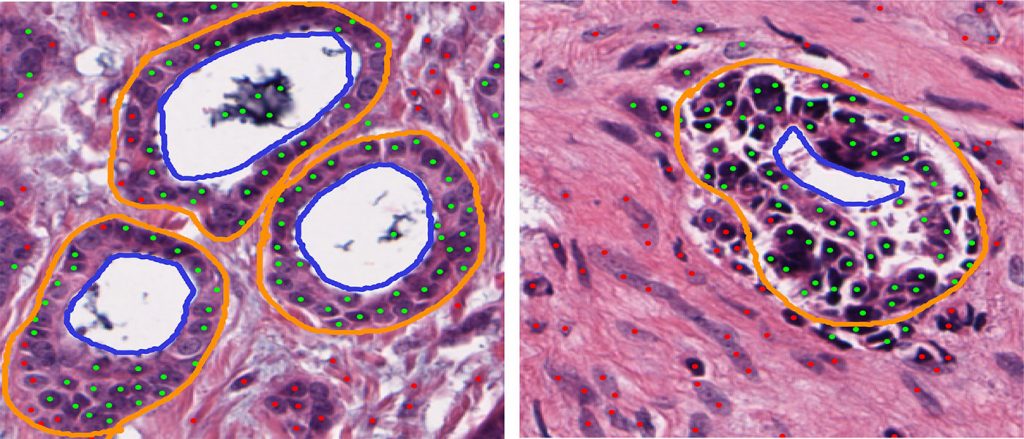
Tubules represent the tumor’s vasculature, providing tumors with oxygen and nutrition. The more of them there are, the more likely a patient will need chemotherapy.
In a study published in Scientific Reports, the researchers developed a computer program to automatically count the number of tubules found in whole slide images of breast cancer tissue specimens. They found the number of tubules correlated with the scores produced by the current best test differentiating between indolent and aggressive ER+ cancers.
“This is the first large-scale validation that fundamental prognostic information is in the tissue data, and that it predicts the underlying genomics of the tumor,” said Anant Madabhushi, F. Alex Nason professor II of biomedical engineering and an author of the study.
“If we can mirror the genomics of the tumor, we can predict who responds to hormone therapy only and who doesn’t,” he said.
Madabhushi teamed with David Romo Bucheli and Eduardo Romero, engineering faculty from the Universidad Nacional de Colombia, in Bogota; Andrew Janowczyk, biomedical engineering research associate at Case Western Reserve; and Hannah Gilmore, associate professor of pathology at Case Western Reserve School of Medicine.
Pathologists currently use three features to grade tumors: mitoses, distinct forms of cell nuclei, called nuclear pleomorphism, and tubules. More of each increases the risk the cancer is aggressive and requires chemotherapy.
The researchers used machine learning to allow a computer to best quantify the number of tubules automatically and quickly.
Using slide images from 174 ER+ patients, they found that the number of tubules correlates with patients’ Oncotype DX gene expression test risk scores.
The gene expression test has been shown to be predictive in identifying which ER+ breast cancer patients would benefit from chemotherapy, but the cost is out of reach for low- and middle-income patients around the world, and the wait time can be weeks, Madabhushi said. His group at the Center for Computational Imaging and Personalized Diagnostics is exploring alternative means to cheaply and quickly provide the same answers.
This study is the first of three by his lab in this area of research. The next quantifies the number of mitoses in whole image slides and correlates the numbers with the genomic test. The last quantifies nuclear pleomorphism and architecture and correlates them with the genomic test.
If all contribute to accurate predictions, Madabhushi plans to integrate them and develop one program that provides a coherent prediction.
This article was originally published Sept. 16.

